Diabetic Kidney Disease (DKD), also known as diabetic nephropathy, is one of the most serious complications of diabetes mellitus. It occurs when long-standing high blood sugar levels damage the kidneys’ filtering units, reducing their ability to remove waste and excess fluids from the body. DKD is a leading cause of chronic kidney disease (CKD) and the most common reason patients progress to end-stage renal disease (ESRD) requiring dialysis or transplantation.
Understanding DKD is important because early detection and treatment can significantly slow its progression, preserve kidney function, and improve quality of life.
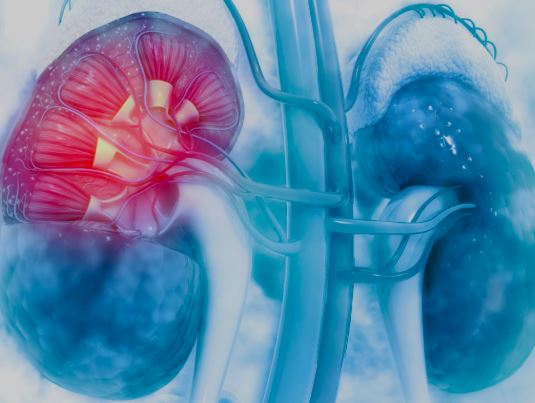
The kidneys are two bean-shaped organs located on either side of the spine, just below the rib cage. Their primary role is to filter blood, removing waste products and balancing fluids, electrolytes, and blood pressure.
Each kidney contains about one million nephrons—tiny filtering units composed of a glomerulus (filter) and a tubule (channel). In diabetic kidney disease, persistent high blood sugar damages the glomeruli, leading to protein leakage into the urine (proteinuria) and a gradual decline in kidney function.
Diabetic kidney disease develops due to a combination of metabolic, hemodynamic, and genetic factors. Key contributors include:
Poorly controlled blood sugar (hyperglycemia): Chronic high glucose damages kidney blood vessels.
High blood pressure (hypertension): Increases stress on delicate kidney filters.
Duration of diabetes: Risk rises with longer duration, especially beyond 10–15 years.
Genetics and family history: Certain individuals are more predisposed.
Other risk factors: Smoking, obesity, high cholesterol, and cardiovascular disease further increase risk.
Diabetic kidney disease often develops silently in its early stages. Symptoms may not appear until significant kidney damage has occurred. Common presentations include:
Early signs:
Protein in urine (microalbuminuria, detectable only by tests)
Swelling in feet, ankles, or hands (edema)
Later symptoms:
Fatigue and weakness
Persistent swelling (legs, face, abdomen)
Increased urination or foamy urine
Nausea, vomiting, or loss of appetite
High blood pressure that is difficult to control
Shortness of breath (due to fluid buildup)
Diagnosis involves a combination of clinical assessment, laboratory tests, and imaging. Key steps include:
History and physical examination – including blood pressure measurement and evaluation of swelling.
Urine tests:
Urine albumin-to-creatinine ratio (UACR) – detects early protein leakage.
24-hour urine protein collection (in select cases).
Blood tests:
Serum creatinine and estimated glomerular filtration rate (eGFR) – to assess kidney function.
Blood glucose and HbA1c – to evaluate diabetes control.
Imaging:
Renal ultrasound may be used to exclude other kidney conditions.
Kidney biopsy (rare): Used when diagnosis is uncertain or if other kidney diseases are suspected.
Treatment aims to slow progression, protect kidney function, and manage complications. There is no permanent cure, but effective measures include:
Blood sugar control:
Insulin therapy or oral antidiabetic medications.
Target HbA1c < 7% (individualized).
Blood pressure control:
ACE inhibitors (e.g., enalapril) or ARBs (e.g., losartan) to protect kidneys.
Goal blood pressure < 130/80 mmHg.
Diet and lifestyle:
Low-salt, moderate-protein diet.
Regular exercise, weight management, and smoking cessation.
Cholesterol management:
Statins to reduce cardiovascular risk.
Newer therapies:
SGLT2 inhibitors (e.g., dapagliflozin) and GLP-1 receptor agonists – shown to benefit kidney outcomes.
In advanced stages (ESRD), when kidneys fail, renal replacement therapy is required:
Hemodialysis – blood filtered through a machine.
Peritoneal dialysis – fluid exchange through the abdomen.
Kidney transplantation – the preferred long-term solution for suitable patients.
Hemodialysis: A vascular access (fistula, graft, or catheter) is created. Blood is drawn, filtered through a dialysis machine, and returned to the body. Typically performed 3 times a week in a hospital or dialysis center.
Peritoneal dialysis: A catheter is inserted into the abdominal cavity. A dialysis solution is infused, absorbs toxins, and then drained. Can be done at home.
Diseased kidney function is replaced by a donor kidney.
Requires surgery under general anesthesia.
Patients must take lifelong immunosuppressive medications to prevent rejection.
Dialysis patients: Regular sessions, strict diet/fluid management, and ongoing monitoring for infection and access site complications.
Transplant patients:
Close follow-up with nephrologists.
Lifelong immunosuppressants.
Regular monitoring of kidney function, infections, and rejection episodes.
Lifestyle measures (healthy diet, exercise, quitting smoking) remain critical.
Potential complications of diabetic kidney disease and its treatments include:
From the disease itself:
Progressive kidney failure
Cardiovascular disease (heart attack, stroke)
Anemia, bone disease, fluid overload
Uremia (toxic buildup of waste)
From treatments:
Side effects of medications (e.g., cough from ACE inhibitors)
Dialysis complications (infection, low blood pressure, clotting of access)
Transplant complications (organ rejection, infections due to immunosuppression)
The outlook depends on stage at diagnosis and control of risk factors.
With early detection and aggressive management, many patients maintain kidney function for decades.
If untreated, DKD typically progresses to end-stage kidney failure within 10–20 years.
Advances in medication, dialysis, and transplantation have significantly improved survival and quality of life.
Patients with diabetes should seek medical attention if they notice:
Swelling of feet, face, or abdomen
Foamy urine or increased urination
Persistent fatigue or unexplained weakness
Uncontrolled blood pressure
Nausea, vomiting, or loss of appetite
Even without symptoms, regular screening (annual urine and blood tests) is essential for all diabetic patients to detect kidney disease early.
Diabetic kidney disease is a common but serious complication of diabetes, with the potential to progress to kidney failure if not managed properly. Through early screening, optimal diabetes and blood pressure control, lifestyle changes, and timely treatment, progression can often be slowed or prevented.
Anyone with diabetes should work closely with their healthcare team, attend regular check-ups, and promptly report any concerning symptoms. Proactive care is the key to preserving kidney health and improving long-term outcomes.
Chat With Me