Glomerular Filtration is the first and most critical step in the process by which the kidneys filter blood and form urine. It refers to the movement of water, electrolytes, and small molecules from the blood into the renal tubules, while larger molecules like proteins and blood cells remain in circulation.
This process is essential for maintaining fluid balance, regulating blood pressure, eliminating waste products, and preserving overall health. Abnormalities in glomerular filtration can indicate or lead to serious kidney diseases, making its understanding vital for both healthcare professionals and patients.
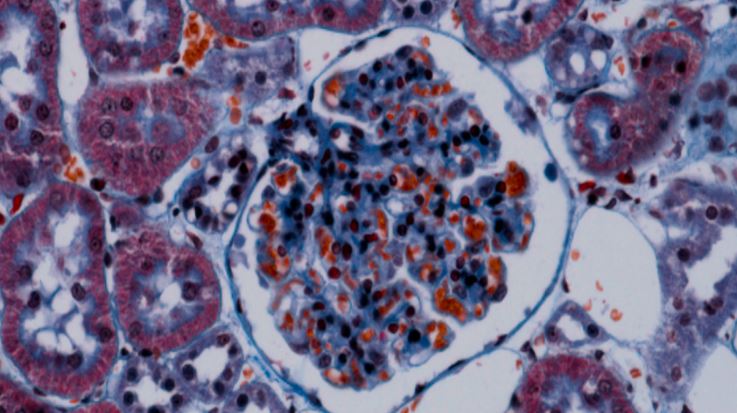
The kidneys contain about 1 million functional units called nephrons, and each nephron has a glomerulus—a tiny cluster of capillaries enclosed in a structure called Bowman’s capsule.
Glomerulus: Acts as a filter, allowing water and small solutes to pass while preventing the loss of proteins and blood cells.
Bowman’s capsule: Collects the filtered fluid (filtrate) that then travels through the renal tubules for further processing.
Glomerular Filtration Rate (GFR): A key measurement of kidney function, indicating how much blood the kidneys filter per minute (normal range is about 90–120 mL/min/1.73m²).
The glomerular filtration barrier has three layers:
Endothelial cells of capillaries (with pores).
Basement membrane (prevents large proteins from passing).
Podocytes (specialized cells with filtration slits).
Together, these structures ensure selective filtration and protect the body from loss of essential proteins and cells.
Disruptions in glomerular filtration may arise due to:
Chronic Kidney Disease (CKD) – Progressive loss of nephron function leading to reduced GFR.
Diabetes Mellitus – High blood sugar damages glomeruli, causing diabetic nephropathy.
Hypertension – Long-term high blood pressure injures delicate glomerular vessels.
Glomerulonephritis – Inflammation of the glomeruli, often due to autoimmune or infectious causes.
Acute Kidney Injury (AKI) – Sudden drop in filtration caused by dehydration, infection, obstruction, or toxins.
Age-related decline – Natural reduction in GFR with aging.
Genetic disorders – Conditions like polycystic kidney disease.
Changes in glomerular filtration may not always present obvious symptoms early on. As kidney function declines, patients may develop:
Swelling in legs, ankles, or around the eyes (edema).
Fatigue and weakness.
Foamy urine (due to protein loss).
Blood in urine (hematuria).
Reduced urine output in severe cases.
Nausea, vomiting, or confusion (in advanced kidney dysfunction).
High blood pressure resistant to medications.
Evaluation of glomerular filtration typically involves both clinical assessment and laboratory tests:
Medical history and examination: Review of risk factors like diabetes, hypertension, or family history.
Blood tests: Measurement of serum creatinine to calculate estimated GFR (eGFR).
Urine tests: Check for proteinuria, hematuria, or abnormal solute levels.
Imaging: Ultrasound or CT to detect structural abnormalities.
Kidney biopsy: Sometimes performed to evaluate underlying glomerular disease.
Regular monitoring of eGFR is crucial for patients at risk of kidney disease.
Treatment depends on the underlying cause of abnormal glomerular filtration.
Non-surgical / medical management:
Blood pressure control with ACE inhibitors or ARBs.
Blood sugar management in diabetic patients.
Immunosuppressive therapy for autoimmune-related glomerulonephritis.
Dietary modifications: Low sodium, protein moderation, and fluid control.
Medications to manage anemia, bone health, or electrolyte imbalances.
Advanced options:
Dialysis (hemodialysis or peritoneal dialysis) when filtration is severely impaired.
Kidney transplantation in end-stage renal disease.
While glomerular filtration itself is not a procedure, interventions like dialysis or kidney transplantation are performed when filtration declines critically:
Dialysis: In hemodialysis, blood is passed through a machine that filters waste before returning it to the body. Peritoneal dialysis uses the abdominal lining as a natural filter.
Kidney Transplant: Involves surgical placement of a healthy donor kidney to restore filtration capacity.
These procedures become essential when natural glomerular filtration is insufficient to sustain health.
For patients undergoing dialysis or kidney transplantation:
Dialysis: Requires regular sessions, dietary restrictions, and infection prevention around vascular access.
Transplant patients: Need lifelong immunosuppressive therapy, close monitoring for rejection, and regular follow-up visits.
Rehabilitation focus: Restoring energy levels, maintaining a kidney-friendly diet, and adherence to medical advice to preserve kidney function.
Disruption of normal glomerular filtration can result in significant complications if untreated:
Fluid overload leading to heart failure or pulmonary edema.
Severe hypertension.
Electrolyte imbalances (dangerous potassium or sodium shifts).
Accumulation of toxins causing uremia.
Increased risk of cardiovascular disease.
Progression to end-stage renal disease (ESRD) requiring dialysis or transplant.
Dialysis and transplantation also carry their own risks, such as infection, clotting, or organ rejection.
The outlook depends on the cause and severity of glomerular filtration impairment:
Mild decline: With proper management, many patients maintain stable kidney function for years.
Moderate to severe decline: Requires careful medical supervision, lifestyle changes, and often long-term treatment.
End-stage disease: Prognosis improves significantly with successful transplantation, while dialysis sustains life but requires continuous management.
Early detection and consistent treatment greatly improve long-term outcomes.
You should seek medical advice if you experience:
Persistent swelling in the legs, face, or around the eyes.
Blood in urine or consistently foamy urine.
High blood pressure not controlled by medications.
Unexplained fatigue, nausea, or reduced urine output.
Family history of kidney disease or existing conditions like diabetes and hypertension.
Glomerular Filtration is the cornerstone of kidney function and overall health. Any disruption can have widespread effects on fluid balance, waste removal, and blood pressure control. Monitoring GFR is one of the best ways to detect kidney disease early and begin timely treatment.
With advances in diagnostics, medical therapy, dialysis, and transplantation, patients with impaired glomerular filtration have more effective treatment options than ever before. If you have risk factors or symptoms suggestive of kidney dysfunction, consult a healthcare professional for proper evaluation and care.
Chat With Me