Fistula and graft placement are critical surgical procedures used to create vascular access for patients undergoing hemodialysis, a life-sustaining treatment for those with end-stage kidney disease. Hemodialysis requires repeated access to the bloodstream to filter waste products and excess fluids, and the quality and durability of this access significantly impact the effectiveness and safety of the treatment. The two primary types of permanent vascular access are arteriovenous (AV) fistulas and AV grafts, each with distinct characteristics, advantages, and considerations.
Hemodialysis involves circulating a patient’s blood through a machine that removes toxins and excess fluids before returning the cleansed blood to the body. To perform this efficiently, a high-flow, durable access point to the bloodstream is necessary. Natural veins are typically too small and fragile to withstand the repeated needle insertions and high blood flow rates required for dialysis. Therefore, surgical creation of an access point that can handle these demands is essential.
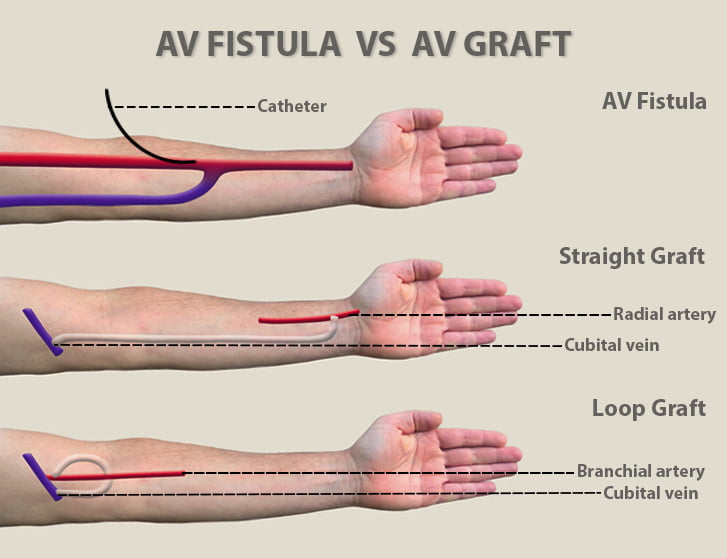
An AV fistula is created by directly connecting an artery to a vein, usually in the forearm or upper arm. This connection causes arterial blood to flow directly into the vein, increasing the vein’s size and wall thickness over time—a process called maturation. The enlarged vein becomes suitable for repeated needle insertions during dialysis.
An AV graft involves implanting a synthetic tube, usually made of polytetrafluoroethylene (PTFE), to connect an artery to a vein. The graft acts as an artificial vein, providing a durable access point for dialysis needles.
Advantages of AV Grafts:
Disadvantages:
The choice between fistula and graft placement depends on multiple factors, including the patient’s vascular anatomy, overall health, and urgency of dialysis initiation. Preoperative evaluation often includes ultrasound mapping of veins and arteries to determine the best site for access creation.
Fistula Creation:
Graft Placement:
After fistula or graft placement, regular monitoring is essential to ensure the access remains functional. This includes physical examination for thrill (a vibration felt over the access), bruit (a sound heard with a stethoscope), and signs of complications such as swelling, redness, or pain.
Common complications include:
Interventional radiology or surgical procedures may be needed to declot or revise the access to maintain its function.
Patients with fistulas or grafts must be educated on how to care for their access site. This includes:
Proper care and timely intervention can prolong the life of the access and reduce complications.
Research continues to improve the materials and techniques used in graft placement, aiming to reduce infection rates and improve durability. Additionally, new surgical methods and imaging technologies help optimize fistula creation and maturation.
Emerging therapies, such as drug-coated grafts and bioengineered vessels, hold promise for enhancing outcomes. Moreover, multidisciplinary care involving nephrologists, vascular surgeons, and interventional radiologists is crucial for managing complex cases and ensuring the best possible patient outcomes.
Fistula and graft placement are foundational procedures for patients requiring hemodialysis. While AV fistulas are preferred due to their longevity and lower complication rates, AV grafts provide a valuable alternative when fistulas are not feasible. Both require careful surgical planning, patient education, and ongoing monitoring to ensure effective and safe dialysis access. Advances in surgical techniques and materials continue to improve the quality of life for patients with kidney failure, making these procedures vital components of renal replacement therapy.
Chat With Me