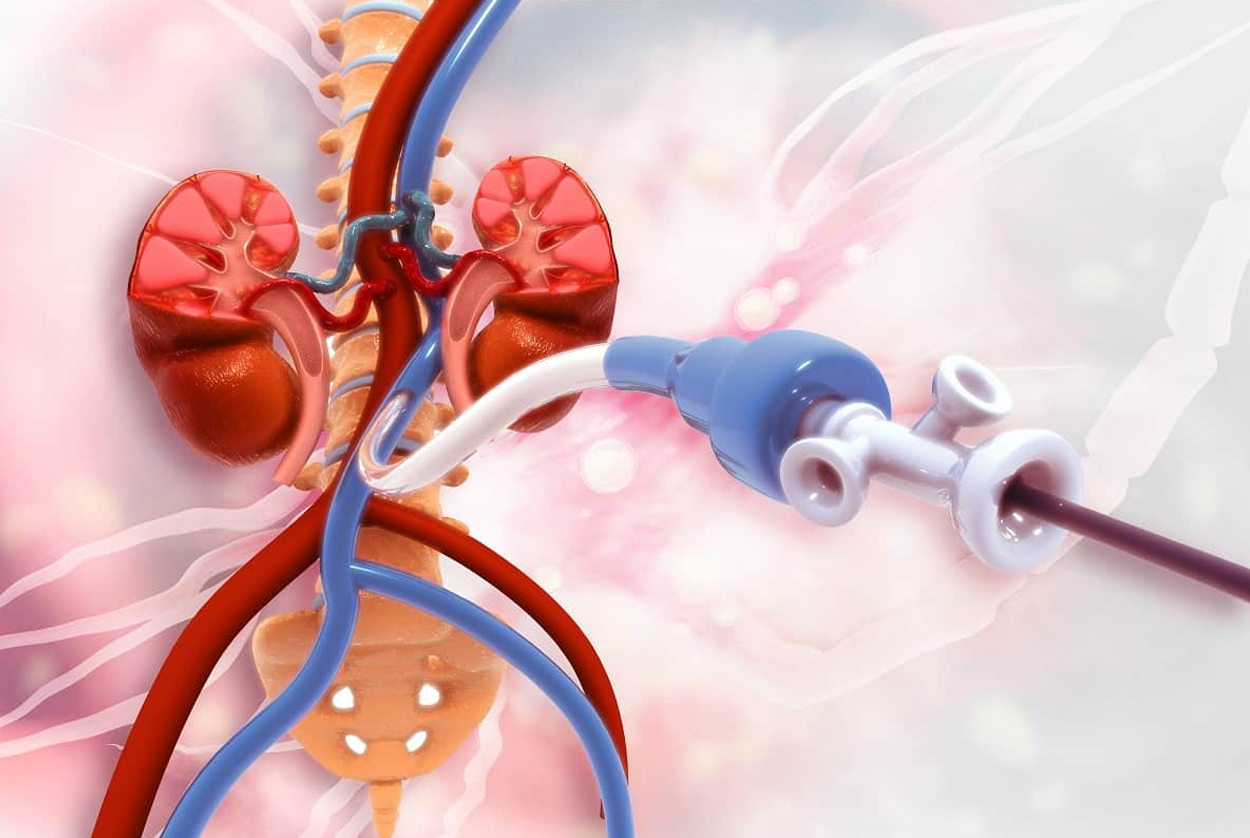
Renal angioplasty is a minimally invasive medical procedure used to treat renal artery stenosis (RAS), a condition characterized by the narrowing of one or both renal arteries, which supply blood to the kidneys. This narrowing can lead to reduced blood flow, causing hypertension (high blood pressure) and potentially leading to kidney damage or failure if left untreated. Renal angioplasty aims to restore adequate blood flow to the kidneys by mechanically widening the narrowed artery, often improving blood pressure control and preserving kidney function.
Renal artery stenosis is most commonly caused by atherosclerosis, a condition where plaque builds up inside the arteries, leading to narrowing and hardening of the vessel walls. Less commonly, fibromuscular dysplasia, a non-atherosclerotic disease affecting the arterial wall, can cause stenosis, especially in younger patients. The reduced blood flow from stenosis triggers the kidneys to release hormones such as renin, which activate the renin-angiotensin-aldosterone system (RAAS), leading to systemic hypertension. This secondary hypertension can be difficult to control with medication alone.
If untreated, renal artery stenosis can cause ischemic nephropathy, a progressive loss of kidney function due to inadequate blood supply. This can eventually lead to chronic kidney disease or end-stage renal failure. Therefore, timely diagnosis and treatment are crucial.
Renal angioplasty is typically indicated in patients with:
The decision to proceed with angioplasty depends on the severity of symptoms, degree of stenosis, and overall patient health.
Renal angioplasty is performed in a catheterization laboratory under fluoroscopic (X-ray) guidance. The procedure involves the following steps:
The entire procedure typically takes one to two hours and is usually done under local anesthesia with sedation.
Renal angioplasty and stenting have been shown to significantly reduce systolic blood pressure in many patients, especially those with severe hypertension related to renal artery stenosis. Improved blood flow to the kidneys can also stabilize or improve kidney function, particularly if the procedure is done before irreversible damage occurs.
Patients often experience a reduction in the number or dosage of antihypertensive medications needed after the procedure. In some cases, blood pressure normalizes completely. Additionally, renal angioplasty can reduce the risk of complications such as heart failure and pulmonary edema associated with renovascular hypertension.
Long-term studies indicate that stenting combined with angioplasty provides better technical success and clinical outcomes compared to angioplasty alone, with lower rates of restenosis.
While renal angioplasty is generally safe, it carries some risks, including:
Contraindications include severe comorbidities that make the procedure unsafe, uncorrectable bleeding disorders, or anatomical factors that preclude safe catheter access.
After renal angioplasty, patients are monitored for complications and kidney function. Blood pressure is regularly checked to assess the effectiveness of the intervention. Antiplatelet medications such as aspirin or clopidogrel are often prescribed to reduce the risk of stent thrombosis.
Follow-up imaging, such as Doppler ultrasound or CT angiography, may be performed periodically to ensure the artery remains open. In some cases, repeat angioplasty may be necessary if restenosis occurs.
Recent advances in catheter technology, imaging, and stent design have improved the safety and efficacy of renal angioplasty. Low-profile balloons and drug-eluting stents are being explored to reduce restenosis rates further.
Despite these advances, the role of renal angioplasty in managing renal artery stenosis remains somewhat controversial. Large clinical trials have shown mixed results regarding its superiority over medical therapy alone, especially in patients with stable kidney function and controlled hypertension. Therefore, patient selection is critical, and the procedure is generally reserved for those who do not respond adequately to medication or who have complications related to renal artery stenosis.
Renal angioplasty is a valuable therapeutic option for patients with significant renal artery stenosis causing hypertension and kidney dysfunction. By mechanically widening the narrowed renal artery and often placing a stent, the procedure restores blood flow, improves blood pressure control, and helps preserve kidney function. While generally safe and effective, careful patient selection and follow-up are essential to optimize outcomes. Advances in technology continue to refine the procedure, making it an important tool in the management of renovascular disease.
Chat With Me