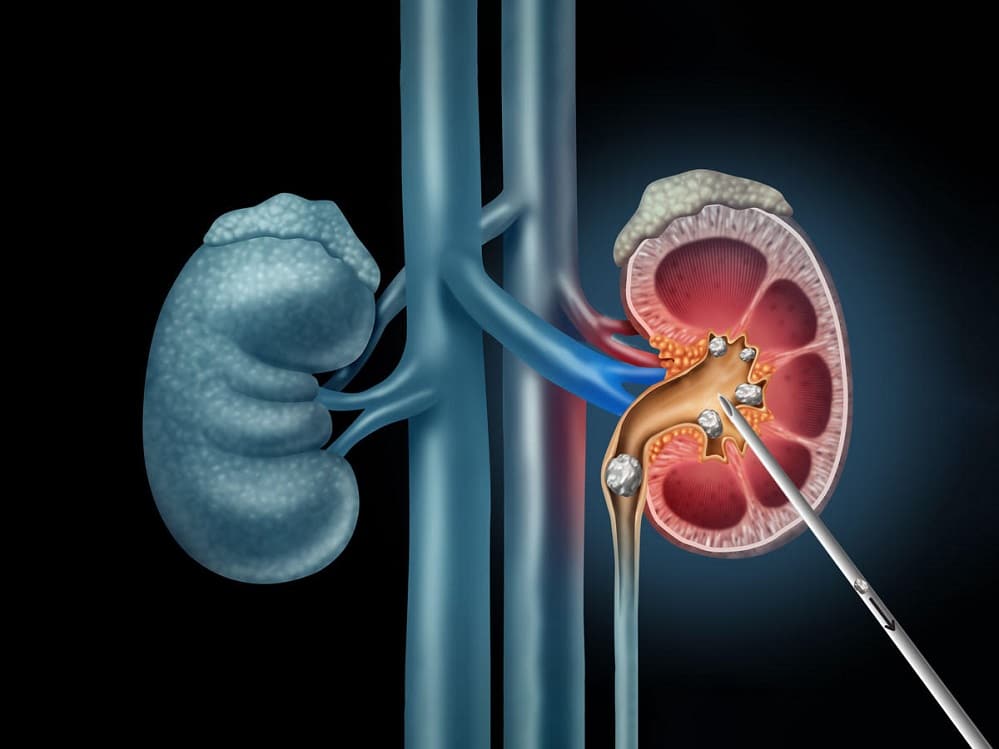
Percutaneous Nephrolithotomy (PCNL) is a minimally invasive surgical procedure designed to remove large or complex kidney stones from the renal pelvis and calyces. First introduced in the late 1970s, PCNL has revolutionized the management of nephrolithiasis, offering a more effective alternative to open surgery for stones that are too big for less invasive methods like extracorporeal shock wave lithotripsy (ESWL) or ureteroscopy. The term “percutaneous” refers to accessing the kidney through the skin, bypassing traditional abdominal incisions. This technique involves creating a tract from the skin to the kidney under imaging guidance, allowing direct visualization and fragmentation of stones using specialized instruments. PCNL is particularly valuable for staghorn calculi—large, branching stones that fill the renal pelvis—or stones greater than 2 cm in diameter, where complete clearance is essential to prevent recurrent infections, obstruction, or kidney damage.
The procedure’s development marked a pivotal shift in urology. In 1976, Japanese urologist Kurth Gerster performed the first percutaneous nephrostomy for drainage, but it was American and European teams in the 1980s who refined it for stone removal. By the 1990s, advancements in endoscopy, fluoroscopy, and ultrasonic lithotripsy tools made PCNL the gold standard for complex cases. Today, it’s performed worldwide, with variations like mini-PCNL or ultra-mini-PCNL adapting the technique for smaller tracts to reduce morbidity.
PCNL is indicated for patients with renal stones that pose significant risks if left untreated. Primary candidates include those with stones larger than 20 mm, as smaller ones can often be managed endoscopically or with shock waves. Staghorn calculi, which can occupy multiple calyces and lead to struvite infections from urease-producing bacteria like Proteus, are a classic indication due to their high recurrence rate—up to 50% without complete removal. Other scenarios include stones causing persistent pain, hematuria, or hydronephrosis (kidney swelling from obstruction), especially in solitary kidneys or when infection is present.
Patient factors play a role too. Those with anatomical challenges, such as horseshoe kidneys or spinal deformities altering pelvic access, may benefit from PCNL’s flexibility. Contraindications are few but include untreated urinary tract infections (to avoid sepsis), uncorrected coagulopathies, or morbid obesity that complicates positioning. Preoperative evaluation is crucial: imaging via non-contrast CT scans assesses stone burden, density (Hounsfield units >1000 indicate harder stones needing PCNL over ESWL), and location. Blood tests check renal function (creatinine, eGFR), coagulation profile, and urine cultures to rule out infection. Patients are often started on antibiotics if cultures are positive.
Preparation begins with multidisciplinary input from urologists, anesthesiologists, and radiologists. Patients undergo a detailed history to identify comorbidities like diabetes or hypertension, which increase perioperative risks. Bowel preparation may be advised to clear the colon, facilitating access to the kidney—typically via a prone position where the 11th intercostal space is punctured. Hydration is encouraged to optimize urine output, and alpha-blockers might be prescribed to relax the ureter if a stent is placed preoperatively.
Informed consent covers potential complications, emphasizing PCNL’s 80-95% stone-free rate for large calculi versus 50-70% for alternatives. For high-risk patients, such as the elderly or those with cardiac issues, supine PCNL (patient on back) is an option to monitor vital signs more easily, though it may limit access.
PCNL is typically performed under general anesthesia in an operating room equipped with fluoroscopy (real-time X-ray) and sometimes ultrasound for guidance. The patient is positioned prone on a radiolucent table, with the affected kidney upward. The goal is to establish a percutaneous tract from the skin to the renal calyx.
Puncture and Tract Dilation: Using intravenous contrast or retrograde pyelography, the collecting system is opacified. A urologist, guided by fluoroscopy, inserts an 18-gauge needle through the skin into a posterior calyx—ideally the lower pole for better drainage. Urine is aspirated to confirm entry, and a guidewire is advanced into the renal pelvis and ureter. The tract is dilated sequentially using balloons or Amplatz dilators up to 24-30 French (Fr) gauge, creating a channel about 8-10 mm wide. A peel-away sheath is placed to maintain access.
Nephroscopy and Stone Fragmentation: A rigid nephroscope (24-32 Fr) is inserted through the sheath, allowing direct visualization of the renal interior via fiberoptic lenses. Stones are engaged with graspers for intact removal if small, or fragmented using ultrasonic, pneumatic (ballistic), or laser lithotripters. For staghorns, multiple accesses might be needed, though single-tract “all-seeing” techniques minimize this. Irrigation fluid (normal saline) flushes fragments, and a nephrostogram checks for residual stones.
Placement of Tube and Closure: Once cleared, a nephrostomy tube (22 Fr) is left in the tract for drainage, connected to a bag. In select cases, “tubeless” PCNL omits the tube, using a ureteral stent instead for faster recovery. The skin puncture is closed with sutures or glue. The procedure lasts 1-3 hours, depending on stone complexity.
Variations include mini-PCNL (14-20 Fr tracts) for smaller stones, reducing bleeding risk, or robotic-assisted PCNL for precision in challenging anatomies. Intraoperative challenges like bleeding from the tract are managed with tamponade or electrocautery.
Postoperatively, patients are monitored in recovery for pain, bleeding (hematuria), and fever. Analgesics (opioids, NSAIDs) control discomfort from the tract, and antibiotics continue for 24-48 hours. The nephrostomy tube drains urine for 1-4 days, with a clamp trial before removal to ensure no obstruction. Hospital stay is 1-3 days, shorter than open surgery’s week-long recovery.
Follow-up includes a low-residue diet to prevent constipation, hydration (2-3 liters/day), and imaging (KUB X-ray or CT) at 4-6 weeks to confirm stone-free status. Patients resume normal activities in 1-2 weeks, avoiding heavy lifting. Long-term, dietary modifications (low oxalate, high citrate) and medications like thiazides prevent recurrence, as 50% of patients may form new stones within 5 years.
PCNL’s advantages are clear: high efficacy (85-95% stone-free for >2 cm stones), single-session treatment for complex cases, and preservation of renal function compared to open surgery. It’s cost-effective long-term by reducing repeat procedures—ESWL often requires multiple sessions with lower success for hard stones.
Disadvantages include its invasiveness relative to endoscopy; it requires general anesthesia and carries higher risks than outpatient options. Radiation exposure from fluoroscopy is a concern, though minimized with ultrasound hybrids.
Complications occur in 10-30% of cases, graded by Clavien system. Minor ones include transient fever (5-10%), pain, or urinary leakage. Major risks: bleeding (1-5% needing transfusion; severe hemorrhage <1% requiring embolization), infection/sepsis (2-5%, potentially fatal in infected systems), pleural injury (hydrothorax if supra-11th rib puncture, 1-3%), or colonic perforation (<1%). Organ injury is rare with proper technique. Mortality is <0.1%, usually from sepsis in frail patients. Risk factors like anticoagulation or large stones are mitigated with careful selection.
Percutaneous Nephrolithotomy (PCNL) stands as a testament to the remarkable progress in minimally invasive urology, transforming the treatment of large and complex kidney stones from high-risk open surgeries to efficient, targeted procedures. With its high stone-free rates—often exceeding 85% for challenging cases—PCNL not only alleviates immediate symptoms like pain and infection but also safeguards long-term renal health, preventing complications such as chronic kidney disease or recurrent obstructions. Despite inherent risks like bleeding or infection, which are mitigated through meticulous patient selection, advanced imaging, and refined techniques, the benefits far outweigh the drawbacks for appropriate candidates.
Chat With Me