Peritoneal dialysis (PD) is a life-sustaining renal replacement therapy for patients with end-stage renal disease (ESRD). Unlike hemodialysis, which filters blood externally, PD utilizes the peritoneal membrane—the thin, semi-permeable lining of the abdominal cavity—as a natural dialyzer. To facilitate this process, a specialized catheter must be surgically inserted into the peritoneal cavity. This procedure, known as peritoneal dialysis catheter insertion, is a critical step that enables the infusion and drainage of dialysate fluid, removing waste products and excess fluid from the body. Performed by trained surgeons or interventional specialists, the insertion bridges the gap between diagnosis and effective dialysis, often allowing patients to manage treatment at home. This article delves into the procedure’s rationale, techniques, preparation, complications, and long-term management, providing a thorough understanding of this essential intervention.
The primary goal of PD is to mimic the kidneys’ filtration function by exploiting osmosis and diffusion across the peritoneum. Dialysate, a sterile glucose-based solution, is introduced into the peritoneal cavity via the catheter, drawing out uremic toxins and water through concentration gradients. Without a reliable catheter, PD is impossible, making insertion a cornerstone of therapy initiation.
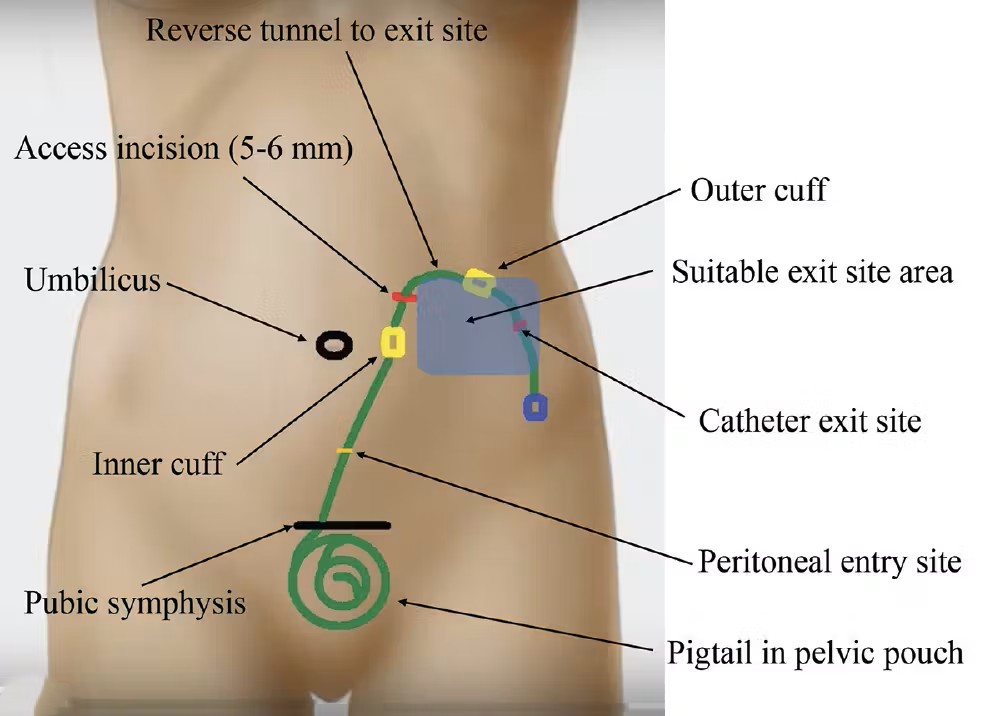
Catheters for PD are designed for durability, biocompatibility, and ease of use. The most common is the Tenckhoff catheter, named after its inventor, Dr. Henry Tenckhoff. Introduced in the 1960s, it features a silicone body with multiple side holes at the distal end for fluid exchange and Dacron cuffs proximally to promote tissue ingrowth, anchoring the device and reducing infection risk. Tenckhoff catheters come in straight, curled ( swan-neck), or pigtail configurations to minimize migration and occlusion.
Other variants include the Toronto-Western catheter, which has a coiled intraperitoneal segment for better fixation, and the Y-tec catheter, emphasizing a pre-sternal exit to lower exit-site infections in obese patients. Single-cuff catheters suit short-term use, while double-cuff models are preferred for long-term PD due to enhanced stability. Material choices, such as medical-grade silicone or polyurethane, prioritize flexibility to prevent kinking while resisting bacterial adhesion.
Selection depends on patient anatomy, PD modality (continuous ambulatory PD or automated PD), and surgeon preference. For instance, curled-tip catheters reduce pain during infusion in patients with a history of abdominal surgeries, where adhesions might complicate straight-tip placement.
Successful catheter insertion begins with meticulous preparation to optimize outcomes and minimize risks. Patients undergo comprehensive evaluation, including medical history review for contraindications like recent abdominal surgery, inflammatory bowel disease, or severe obesity, which could impair peritoneal function. Imaging, such as ultrasound or CT scans, assesses the peritoneal cavity for adhesions or hernias. Blood tests evaluate coagulation status, as bleeding risks are heightened in uremic patients.
Antibiotic prophylaxis is standard to prevent peritonitis, the most dreaded complication. Typically, a first-generation cephalosporin like cefazolin is administered intravenously 30-60 minutes pre-procedure. Patients are advised to fast for at least six hours, and bowel preparation with laxatives may be used to clear the intestines, ensuring a sterile field.
Informed consent is crucial, discussing benefits—such as home-based dialysis preserving residual kidney function and offering lifestyle flexibility—against risks like infection (up to 20% in the first year), bleeding, or bowel perforation (rare, <1%). Psychological support addresses anxiety, as PD demands patient involvement in daily exchanges.
The procedure is often scheduled electively, ideally 2-4 weeks before dialysis initiation to allow a “break-in” period for healing. In urgent cases, temporary hemodialysis bridges the gap.
Catheter insertion techniques vary by setting, patient condition, and institutional resources, balancing efficacy with minimal invasiveness. The three main approaches are open surgical, laparoscopic, and percutaneous (Seldinger technique).
This traditional method involves a 5-7 cm midline incision below the umbilicus under general or local anesthesia with sedation. The peritoneum is directly visualized and accessed, allowing careful dissection to create a tunnel for the catheter. The distal tip is positioned in the true pelvis to optimize dialysate distribution and drainage, avoiding the omentum. The proximal end exits laterally, typically in the right lower quadrant, with cuffs buried subcutaneously for 2-4 cm to foster fibrosis.
Advantages include direct visualization, ideal for complex anatomies like prior surgeries. However, it requires a larger incision, increasing pain and recovery time (1-2 weeks). Operative time is 30-60 minutes, with hospital stays of 1-3 days.
Gaining popularity, laparoscopy uses small ports (5-10 mm) and a camera for minimally invasive placement. Under general anesthesia, CO2 insufflation creates a pneumoperitoneum, enabling inspection for adhesions. The catheter is advanced through a trocar, secured with omentopexy (suturing omentum away from the tip) if needed, and tunneled externally.
This approach reduces postoperative pain, shortens hospital stays (often outpatient), and lowers hernia risk by allowing concurrent hernia repairs. Complication rates are comparable to open surgery but with better cosmesis. It’s particularly beneficial for patients with obesity or prior laparotomies, though it demands advanced laparoscopic skills and equipment.
A bedside option using the Seldinger technique, this mirrors central line placement. Under local anesthesia and ultrasound guidance, a needle punctures the peritoneum, a guidewire is advanced, and the catheter is dilated and inserted over it. Fluoroscopy may confirm tip position.
It’s quick (15-30 minutes) and cost-effective, suitable for low-risk patients without adhesions. However, blind insertion raises perforation risks (up to 5%), making it less ideal for those with abdominal scars. Success rates exceed 90% in experienced hands.
Regardless of method, hemostasis is ensured, and the exit site is dressed sterilely. Immediate post-op, a small-volume dialysate dwell (e.g., 500 mL) tests patency and leaks.
Post-insertion management focuses on healing and infection prevention. Patients receive analgesics, antibiotics for 24-48 hours, and immobilization to avoid dislodgement. The exit site is cleaned daily with chlorhexidine, and dressings changed under aseptic conditions. Heparin or citrate may flush the catheter to prevent fibrin clots.
The break-in period, lasting 2-6 weeks, allows cuff integration and reduces leak risk. During this time, low-volume dwells (1-1.5 L) are performed intermittently, avoiding full PD cycles. Patients learn catheter care through training programs, covering connection to cyclers, hygiene, and troubleshooting.
While effective, insertion carries risks. Early complications include bleeding (1-2%), managed conservatively or surgically; exit-site infections (10-15%), treated with topical antibiotics; and pericatheter leaks, resolved by temporary PD cessation.
Peritonitis, often from touch contamination, presents with cloudy effluent and fever, requiring prompt intraperitoneal antibiotics. Late issues encompass catheter migration (5-10%), causing poor drainage—repositioned via interventional radiology—or occlusion by fibrin/plaque, addressed with thrombolytics or replacement.
Infection rates have declined with standardized protocols, but overall, 20-30% of catheters require removal within two years. Patient factors like diabetes increase vulnerability, underscoring the need for multidisciplinary care involving nephrologists, surgeons, and nurses.
Long-term success hinges on adherence. PD preserves vascular access for potential future hemodialysis and offers superior quality of life, with studies showing better anemia control and fewer dietary restrictions. Catheter survival averages 2-3 years, with survival rates of 80% at one year and 50% at five years.
Innovations like antimicrobial-coated catheters and embedded sensors for infection detection promise further improvements. For patients, insertion marks empowerment, transitioning from hospital dependency to self-managed care.
In conclusion, peritoneal dialysis catheter insertion is a pivotal procedure blending surgical precision with patient-centered care. By addressing anatomical challenges and infection risks, it enables effective PD, extending life and enhancing autonomy for ESRD patients. Ongoing research refines techniques, ensuring this therapy remains a viable, home-friendly option in the dialysis landscape.
In conclusion, peritoneal dialysis catheter insertion is a pivotal procedure blending surgical precision with patient-centered care. By addressing anatomical challenges and infection risks, it enables effective PD, extending life and enhancing autonomy for ESRD patients. Ongoing research refines techniques, ensuring this therapy remains a viable, home-friendly option in the dialysis landscape.
Chat With Me