Kidney transplantation is often considered the best treatment for patients with end-stage renal disease (ESRD), offering improved survival and quality of life compared to long-term dialysis. However, like all major medical procedures, transplantation carries risks. Post Kidney Transplant Complications can arise immediately after surgery or years later, affecting graft function and overall patient health.
Understanding these complications is crucial for patients, caregivers, and healthcare providers. With timely recognition, appropriate treatment, and regular follow-up, many complications can be managed successfully, ensuring long-term graft survival and improved patient outcomes.
The kidneys are vital organs responsible for filtering waste products, balancing electrolytes, regulating blood pressure, and producing certain hormones. In a kidney transplant, a healthy donor kidney is surgically placed into a recipient whose kidneys are no longer functioning adequately.
The donor kidney is usually placed in the lower abdomen (iliac fossa).
The renal artery and vein of the donor kidney are connected to the recipient’s iliac vessels.
The ureter (tube carrying urine) is attached to the bladder to allow urine drainage.
Because the transplanted kidney is a foreign organ, the recipient’s immune system may recognize it as “non-self” and attempt to reject it. To prevent this, patients require lifelong immunosuppressive medications, which carry their own risks.
Post-transplant complications arise due to multiple factors, including:
Immune response – The body’s defense system may attack the donor kidney, leading to rejection.
Infections – Immunosuppressive therapy increases susceptibility to bacterial, viral, and fungal infections.
Medication side effects – Long-term immunosuppressants can cause kidney toxicity, diabetes, hypertension, and bone disease.
Surgical complications – Technical issues such as blood clots, ureteral leaks, or vascular problems.
Underlying patient conditions – Diabetes, hypertension, or cardiovascular disease may complicate recovery.
The symptoms of post-kidney transplant complications vary depending on the type of problem:
Rejection: Fever, decreased urine output, swelling, weight gain, pain over the graft site, and rising serum creatinine.
Infection: Fever, chills, burning during urination, cough, or general malaise.
Medication toxicity: High blood pressure, tremors, or abnormal lab results (elevated creatinine, abnormal electrolytes).
Surgical complications: Abdominal pain, swelling, blood in urine, or urine leakage.
Chronic issues: Fatigue, persistent hypertension, bone pain, or recurrent urinary tract infections.
Any new or unexplained symptom in a transplant patient should be taken seriously and evaluated promptly.
Diagnosing post-transplant complications involves a combination of clinical evaluation, laboratory tests, and imaging studies:
Blood tests: Serum creatinine, blood urea nitrogen (BUN), electrolytes, and drug levels to assess kidney function and medication toxicity.
Urine tests: Urinalysis and cultures to check for infection or protein leakage.
Imaging: Ultrasound and Doppler studies to assess blood flow, obstruction, or fluid collections.
Kidney biopsy: Gold standard for diagnosing rejection, providing microscopic evidence of immune-mediated damage.
Viral load testing: For infections like cytomegalovirus (CMV) or BK virus.
Treatment depends on the complication identified:
Rejection:
Acute rejection: High-dose corticosteroids or additional immunosuppressants (e.g., anti-thymocyte globulin).
Chronic rejection: Often irreversible, managed by optimizing immunosuppression and controlling risk factors.
Infections:
Antibiotics, antivirals, or antifungals depending on the pathogen.
Dose adjustment of immunosuppressive drugs may be necessary.
Medication side effects:
Dose modification or switching to alternative drugs.
Supportive management for hypertension, diabetes, or osteoporosis.
Surgical complications:
Minor issues may be managed conservatively.
Severe complications may require corrective surgery.
If surgical intervention is required for complications, common procedures include:
Revision of vascular anastomosis to correct clotting or poor blood flow.
Ureteral reconstruction to address leaks or strictures.
Drainage of fluid collections (hematoma, lymphocele, or abscess).
Graft nephrectomy (removal of transplanted kidney) in severe cases of infection or irreversible rejection.
These procedures are usually performed under general anesthesia, with patients closely monitored during recovery.
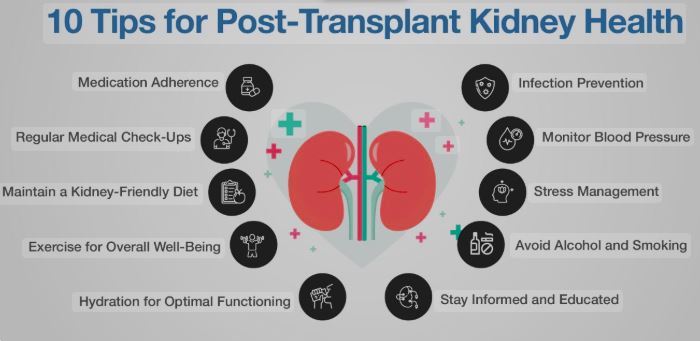
Recovery after Kidney transplant and management of complications requires lifelong commitment:
Regular follow-up: Frequent blood tests and clinic visits, especially in the first year.
Medication adherence: Strict compliance with immunosuppressive therapy.
Infection prevention: Vaccinations, hand hygiene, and avoiding exposure to contagious individuals.
Lifestyle modifications: Balanced diet, regular exercise, weight control, and avoiding smoking or excessive alcohol.
Psychological support: Coping with long-term treatment and lifestyle changes can be challenging.
Some of the most common post-transplant complications include:
Acute or chronic rejection.
Infections: Urinary tract infections, pneumonia, CMV, or BK virus.
Cardiovascular disease: Leading cause of long-term mortality in transplant patients.
Post-transplant diabetes mellitus.
Cancer: Increased risk due to long-term immunosuppression (e.g., skin cancers, lymphomas).
Bone disease: Osteoporosis or fractures due to steroids.
Medication-related toxicity: Nephrotoxicity, liver dysfunction, or gastrointestinal problems.
With modern surgical techniques and effective immunosuppressive therapy, outcomes of kidney transplantation are generally excellent.
1-year graft survival rates exceed 90% in most centers.
Many patients enjoy normal or near-normal kidney function for 10–20 years or more.
Long-term survival depends on adherence to medications, control of comorbidities, and early detection of complications.
Despite risks, kidney transplantation significantly improves quality of life compared to dialysis, allowing patients to work, travel, and live more independently.
Patients should seek immediate medical care if they experience:
Reduced urine output or dark urine.
Swelling in the legs, ankles, or around the eyes.
Pain or tenderness at the graft site.
Persistent fever, cough, or unexplained fatigue.
Sudden weight gain or uncontrolled blood pressure.
Any signs of infection (burning urination, chills, sore throat).
Prompt evaluation can prevent serious complications and protect the transplanted kidney.
Kidney transplantation offers a new lease on life for patients with end-stage renal disease, but it also comes with potential risks. Post Kidney Transplant Complications can occur early or late, ranging from surgical problems and infections to rejection and medication side effects.
The key to long-term success is vigilance—through regular follow-up, adherence to medications, healthy lifestyle choices, and open communication with healthcare providers. With proper care and early intervention, most complications can be managed effectively, ensuring the transplanted kidney continues to function for many years.
Chat With Me