Pyelonephritis is a type of urinary tract infection (UTI) that specifically affects the kidneys. It is an inflammation of the kidney tissue and renal pelvis, usually caused by bacterial infection, though viruses can also be responsible in some cases. This condition can affect one or both kidneys and is considered more serious than lower urinary tract infections, such as cystitis, because it involves the upper urinary tract and can lead to significant complications if not treated promptly.
The most common cause of pyelonephritis is a bacterial infection, typically by Escherichia coli (E. coli), which normally resides in the intestines. These bacteria can enter the urinary tract through the urethra and ascend to the bladder, causing cystitis, and then continue upward to infect the kidneys. Other bacteria such as Klebsiella, Proteus, Enterobacter, and Pseudomonas species can also cause pyelonephritis, especially in hospital-acquired infections or in patients with structural abnormalities of the urinary tract.
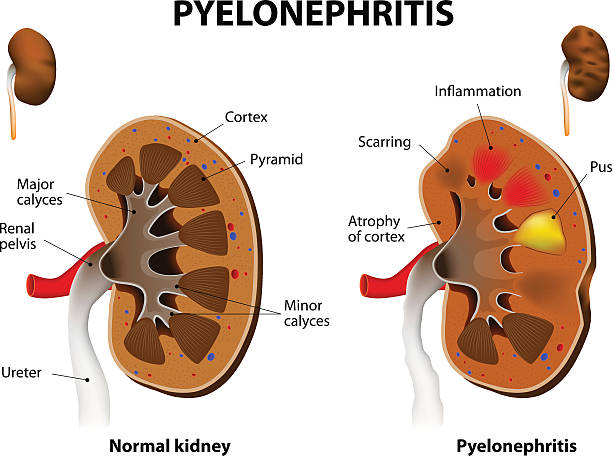
The infection usually begins in the lower urinary tract and ascends to the kidneys via the ureters. In some cases, bacteria can reach the kidneys through the bloodstream, especially in patients with compromised immune systems or systemic infections. Once bacteria reach the kidneys, they cause inflammation and swelling of the renal parenchyma and pelvis, which can impair kidney function.
Certain factors increase the risk of developing pyelonephritis, including urinary tract obstruction (such as kidney stones or an enlarged prostate), vesicoureteral reflux (a condition where urine flows backward from the bladder to the kidneys), diabetes, pregnancy, immunosuppression, and the presence of urinary catheters.
The symptoms of pyelonephritis are often more severe than those of lower urinary tract infections. Common signs include:
In severe cases, pyelonephritis can lead to sepsis, a life-threatening systemic infection, especially if the infection spreads beyond the kidneys.
Diagnosis of pyelonephritis is based on clinical presentation, physical examination, and laboratory tests. A healthcare provider will typically look for signs such as fever, flank tenderness (pain when pressing on the sides of the lower back), and symptoms of urinary tract infection.
Laboratory tests include:
Prompt treatment of pyelonephritis is essential to prevent kidney damage and systemic complications. The mainstay of treatment is antibiotics, which are chosen based on the likely causative bacteria and local antibiotic resistance patterns.
In cases where an underlying cause such as urinary obstruction or kidney stones is identified, addressing these issues is crucial to prevent recurrent infections.
If left untreated or inadequately treated, pyelonephritis can lead to serious complications, including:
Preventing pyelonephritis involves reducing the risk of urinary tract infections and addressing predisposing factors:
Pyelonephritis is a serious kidney infection that requires timely diagnosis and treatment to prevent complications. It typically arises from bacterial infections ascending from the lower urinary tract and presents with fever, flank pain, and urinary symptoms. Diagnosis involves clinical evaluation and laboratory testing, while treatment centers on appropriate antibiotics and supportive care. Awareness of risk factors and preventive measures can help reduce the incidence of this potentially severe condition.
Chat With Me